Slip disc is such a commonly heard term among back pain sufferers. Already about 70% of the Indian Population is reported to have suffered from back pain at least once during their lifetime. Slip disc or disc protrusion or PIVD makes the largest chunk among the possible cause for this LBP.
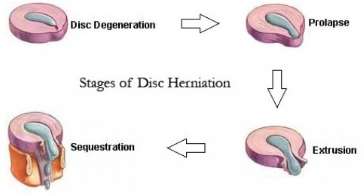
As we age the discs that are present in our vertebral column, become less flexible and begin to harden, making them more prone to tears. A herniated disc can be caused by a single excessive strain or injury. However, as degeneration of the discs progresses with age, some people may suffer herniated discs from more minor exertions or twists.
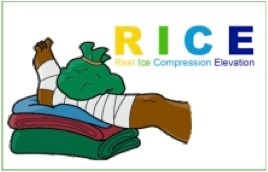
The first line of treatment, if you have recently had a slipped disc
Immediately after having an episode of PIVD, care should be taken to:
- Stop the offending /painful movements and activities
- Lying on your back with feet on a chair & knees at a 90-degree angle can sometimes be quite comfortable for the back.
- Apply a cold pack at least 4-5 times a day for 10 minutes at a time
- See a health care provider (Physiotherapist/orthopedic) assess the causes and understand your pain clinically
What are the treatment options for a Prolapsed Disc?
Treatment of a PIVD depends on the level of severity and discomfort you are facing and how far the disc has slipped out of its place. Usually, the line of treatment includes:
Local pain relief: Muscle relaxants or analgesics or non-steroidal anti-inflammatory drugs under the ortho’s prescription can be useful.
Physiotherapy – Once the initial inflammation has settled, an appropriate physiotherapy program can relieve the pain. A Physiotherapist will also prescribe an exercise program that strengthens the core and other involved structures.
Surgery – Severe nerve entrapments may require minor surgeries like microdiscectomy.
Tips to manage Prolapsed disc at home
In spite of the line of treatment you choose for slipped disc, you still need to consider the following tips to manage PIVD better:
Sit for an only a short period of time
– Your back wants movement and sitting in a chair for an extended period of time puts your back into a loaded flexed position, which your spine will not like. Try to change positions every 30-40 minutes by standing up, going for a little walk, or grabbing a glass of water. While you are sitting for short periods, you want to make sure you sit with good posture and proper lumbar (lower back) support.
Apply heat to the affected area
By using heat you are helping to decrease muscle spasms and improve blood flow through the body. Try using a hot water bottle for 10 minutes or as often as required. Just be sure to place something between your skin and the heat pack to prevent any skin burns.
In case there is swelling or localized warmth, use an ice pack for 10 minutes. Read more about using heat and ice.
Find a comfortable sleeping position
It is important to sleep with proper support so if you like to sleep on your side, place a pillow between your legs to take off any extra pressure through your hips and lower back. If you prefer sleeping on your back, place a pillow or rolled-up towel underneath your knees so they are propped up allowing your lumbar spine to relax in a neutral position. These small modifications can help ease any pressure on your spine
Healthy exercise lifestyle
Most importantly, continue your exercise program as a part of maintenance and do regular follow-ups with your physiotherapist.
Find a comfortable sleeping position
It is important to sleep with proper support so if you like to sleep on your side, place a pillow between your legs to take off any extra pressure through your hips and lower back. If you prefer sleeping on your back, place a pillow or rolled-up towel underneath your knees so they are propped up allowing your lumbar spine to relax in a neutral position. These small modifications can help ease any pressure on your spine
Healthy exercise lifestyle
Most importantly, continue your exercise program as a part of maintenance and do regular follow-ups with your physiotherapist.
How does Physiotherapy help in treating Prolapsed discs?
Physiotherapy provides successful treatment for spinal disc prolapse rehabilitation. Typically the treatment includes back pain relief and protection, an exercise program for lower abdomen and core stability, restoration of function, and preventing a recurrence.
RehabMax Physiotherapy provides Disc prolapse rehabilitation for managing such symptoms at its clinics in Howrah, Kolkata. The treatment phases are described hereunder:
A.Back Pain Relief & Protection:
Our physiotherapists will use an array of treatment tools to reduce your back pain and inflammation. These include ice, electrotherapy, and unloading taping techniques. Apart from these certain techniques or exercises that unload the inflamed structures are also utilized to provide pain relief and reduce inflammation.
B.Prolapsed Disc Exercises:
- As your pain and inflammation settle, our physiotherapist will turn their attention to restoring your normal joint alignment and range of motion, muscle length and resting tension, muscle strength, and endurance.
- Our physiotherapist will commence you on a lower abdominal and core stability program to facilitate your important muscles that dynamically control and stabilize your spine.
- Our physiotherapist may recommend a stretching program to address your tight or shortened muscles.

C.Restoring Full Function:
Depending on your chosen work, sport, or activities of daily living, our physiotherapist will aim to restore your function to safely allow you to return to your desired activities. Everyone has different demands for their body that will determine what specific treatment goals you need to achieve. For some, it is simply to walk around the block. Others may wish to run a marathon.
Your physiotherapist will tailor your back rehabilitation to help you achieve your own functional goals.
D.Preventing a Recurrence:
Back pain does have a tendency to return. The main reason it is thought to recur is due to insufficient rehabilitation. In particular, poor compliance with deep abdominal and core muscle exercises. You should continue a version of these exercises routinely a few times per week.
What is Prolapsed disc or PIVD?
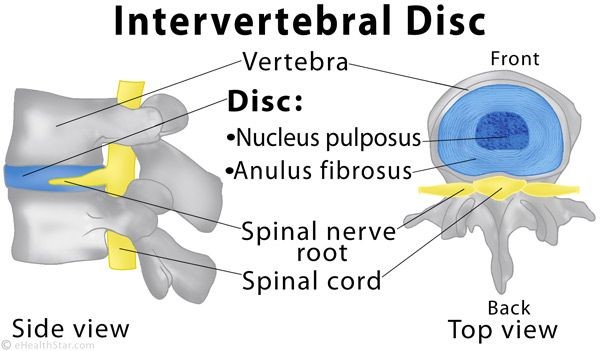
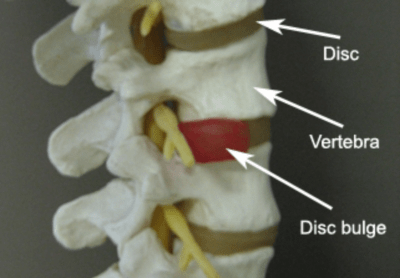
To understand Prolapsed Intervertebral Disc (PIVD), also known as a herniated disc or disc protrusion or disc prolapsed; it is important to understand the central structure of our disc.
A prolapsed /herniated disc means the displacement of the content of the disc beyond its boundaries into the intervertebral space. Your disc is made up of 2 layers- a thick outer layer called Annulus Fibrosus and the soft gel-like center called Nucleus Pulposus.
You can relate this stricture to a cream biscuit. The biscuits as the tough outer layer annulus and the cream is the central gel-like structure nucleus.
These discs act as cushions or shock absorbers between the vertebras.
PIVD is actually an age-related problem. But trauma, strains, torsion, or heavy lifting can cause disc prolapse/herniations. It can occur in any disc of the spine but lumbar (lower back) and cervical (neck) disc prolapses are common forms.
What are the causes of Disc Prolapse?
Pain caused due to disc prolapse/ herniation may seem to occur suddenly but it is usually a result of a gradual process accumulating due to many of the following causes:
- Aging
- Being overweight (creating more pressure on the spinal column)
- Smoking (which can contribute to the degeneration of discs)
- Incorrect lifting of heavyweights.
- Repetitive strenuous activity.
- Less common causes would be traumatic injuries like a fall or an accident that puts pressure on the disc and causes its displacement.
What are the signs and symptoms of prolapsed disc?
The most common symptom of a herniated disc are:
- Pain &/or numbness
- Pain that extends to the arms from your neck OR pain that extends to the legs from the lower back (sciatica pain)
- Pain worsening at night while asleep or with certain activities that defines the pressure on your discs
- Pain worsening on standing/sitting
- Pain on walking specific distances
- Muscle weakness in a higher degree of disc involvement
- Tingling, aching, or burning sensation in the affected area
- The type of pain or symptoms may vary from person to person depending on the severity of disc involvement.
If problems with bowel or bladder function are experienced this may be a sign of cauda equine syndrome – a rare but serious complication of a herniated disc. Immediate medical attention should be sought if this is suspected.

How much time does it take to recover from prolapsed disc?
Your discs do not have a blood supply (blood is what brings the healing to any damaged structure). This means that your disc doesn’t have any repairing powers of its own and if injured, your spinal disc cannot repair itself.
After a disc injury, your disc would undergo the following 3 stages:
- Significant dysfunction due to pain
- The long phase of instability makes you more prone to back pain episodes
- The body tries to re-stabilize the segment and you may have lesser episodes of pain.
- Either way, a physiotherapist at ReLiva will plan your treatment based on your assessment and your recovery stage. The time frame of recovery varies
- based on the severity of structural involvement. But in general, your recovery stages would be as follows :
1. Acute inflammatory stage
– in this stage, your pain has just started but is very severe in nature and constantly present. No movement or position helps you relieve the symptom.
2. Acute stage without inflammation
– here the symptoms are intermittent in nature and usually related to offending activities or movements.
For eg: if you cannot stand longer than 15 min/sit longer than 30 min/walk for more than a mile. Attempting these activities beyond your mechanical limits will aggravate your pain symptoms.
3. Subacute stage
– usually at this stage, certain movements & postures still provoke the pain.
4. Chronic stage
– when this stage is reached, emphasis is placed on returning the highest level of activity that requires you to perform a repeated movement or we can say repeated loading. For eg: lifting something or playing a sport etc.
What are the complications of a Prolapsed disc?
An untreated slipped disc can manifest in various ways:
- An untreated, severe slipped disc can lead to permanent nerve damage.
- In very rare cases, a slipped disc can cut off nerve impulses to the end of the spinal column called as cauda equina in your lower back and legs. If this occurs, you may lose bowel or bladder control.
- Another long-term complication is known as saddle anesthesia. In this case, the slipped disc compresses nerves and causes you to lose sensation in your inner thighs, the back of your legs, and around your rectum.
- While the symptoms of a slipped disc may improve, they also can worsen. If you cannot perform the activities you once could, it’s time to see your doctor.
Frequently asked Questions – FAQs for prolapsed disc